Individuals differ in their susceptibility to viral infections and genes contribute to the risk score. Less than 10% of humans infected with Mycobacterium tuberculosis develop TB, partially because of polymorphism in Tyrosine kinase (TYK2, P1104A) also responsible for severe COVID-19. Early in the pandemic, it was discovered that SARS-CoV-2 infection is dependent on the ACE2 receptor for cell entry and the serine protease TMPRSS2 for spike protein priming. ACE2 expression, indeed, influences COVID-19 risk and a rare variant located close to this gene was found to confer protection against COVID-19, possibly by decreasing ACE2 expression. Interestingly, FMO3 is one of the few genes with expression correlated to ACE2 [Sungnak et al, 2020] along with genes associated with immune functions.
One of the characteristics of COVID-19 is the appearance of inflammatory processes, which could be leading to increased levels of TMAO. It could contribute to the hypercoagulative state in COVID-19-associated coagulopathy (CAC). SARS-Cov2 was shown to enhance TMAO-induced inflammation.
Coronavirus disease is associated with increased risk of thrombotic events. According to recent research, low levels of FMO3 protect against thrombosis [Shih et al, 2019] while some FMO3 mutations confer higher risk [Oliveira-Filho et al, 2021]. FMO3 rs1736557 might increase the anti‐platelet efficacy of clopidogrel [Zhu et al, 2021]. Genetic risk can be mediated by gut microbiota [Gabashvili, 2020]. There are also associations with salt tolerance, wound healing, and diseases such as diabetes, renal and cardiovascular conditions increasing risk of severe COVID-19.
Studying trimethylaminuria-like conditions might help in developing strategies for prevention and therapy of other diseases, including COVID-19.
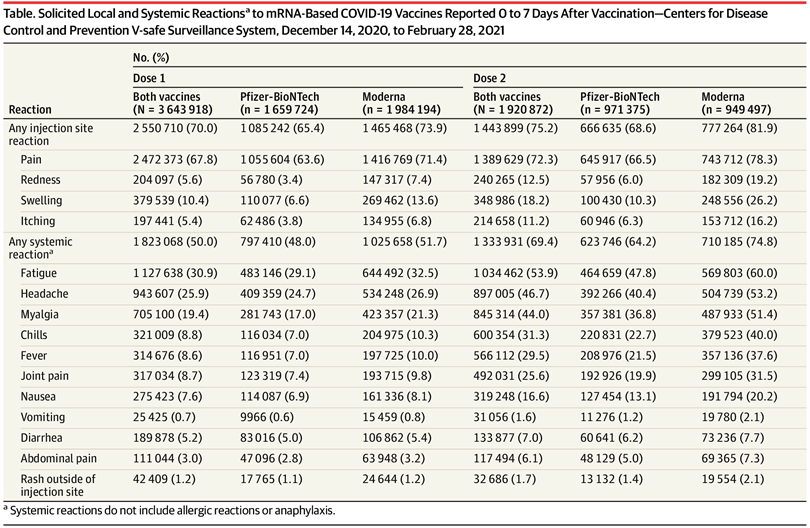
Our COVID-19 disease and vaccines study [NCT04832932, Gabashvili, 2021] compares side-effects of vaccines and clinical course of infections (including vaccine breakthroughs) in several cohorts including MEBO and TMAU. You can help by enrolling and participating in this online survey in English or Spanish.
REFERENCES
Andreakos E, Abel L, Vinh DC, Kaja E, Drolet BA, Zhang Q, O’Farrelly C, Novelli G, Rodríguez-Gallego C, Haerynck F, Prando C. A global effort to dissect the human genetic basis of resistance to SARS-CoV-2 infection. Nature immunology. 2021 Oct 18:1-6.
Gabashvili IS. Cutaneous Bacteria in the Gut Microbiome as Biomarkers of Systemic Malodor and People Are Allergic to Me (PATM) Conditions: Insights from a Virtually Conducted Clinical Trial. JMIR Dermatology. 2020 Nov 4;3(1):e10508.
Gabashvili IS. Community-Based Phenotypic Study of Safety, Tolerability, Reactogenicity and Immunogenicity of Emergency-Use-Authorized Vaccines Against COVID-19 and Viral Shedding Potential of Post-Vaccination Infections: Protocol for an Ambispective study. medRxiv 2021.06.28.21256779; doi: https://doi.org/10.1101/2021.06.28.21256779
Liu W, Wang C, Xia Y, Xia W, Liu G, Ren C, Gu Y, Li X, Lu P. Elevated plasma trimethylamine-N-oxide levels are associated with diabetic retinopathy. Acta Diabetologica. 2021 Feb;58(2):221-9.
Janmohamed A, Dolphin CT, Phillips IR, Shephard EA. Quantification and cellular localization of expression in human skin of genes encoding flavin-containing monooxygenases and cytochromes P450. Biochemical pharmacology. 2001 Sep 15;62(6):777-86.
Oliveira-Filho AF, Medeiros PF, Velloso RN, Lima EC, Aquino IM, Nunes AB. Trimethylaminuria and Vascular Complications. Journal of the Endocrine Society. 2021 Apr;5(Supplement_1):A313-4.
Zhu KX, Song PY, Li MP, Du YX, Ma QL, Peng LM, Chen XP. Association of FMO3 rs1736557 polymorphism with clopidogrel response in Chinese patients with coronary artery disease. European Journal of Clinical Pharmacology. 2021 Mar;77(3):359-68.
Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, Talavera-López C, Maatz H, Reichart D, Sampaziotis F, Worlock KB. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nature medicine. 2020 May;26(5):681-7.
Shih, D.M., Zhu, W., Schugar, R.C., Meng, Y., Jia, X., Miikeda, A., Wang, Z., Zieger, M., Lee, R., Graham, M. and Allayee, H., 2019. Genetic deficiency of Flavin-containing monooxygenase 3 (Fmo3) protects against thrombosis but has only a minor effect on plasma lipid levels—brief report. Arteriosclerosis, thrombosis, and vascular biology, 39(6), pp.1045-1054.