Despite being the overlooked Cinderella of our senses, the impact of smell on our well-being is profound.
Tuesday, December 20, 2022
Current Trends in Deodorization
Thursday, November 17, 2022
Olfactory Signatures and COVID-19
REFERENCE
Gabashvili IS. The Incidence and Effect of Adverse Events Due to COVID-19 Vaccines on Breakthrough Infections: Decentralized Observational Study With Underrepresented Groups. JMIR Formative Research. 2022 Nov;6(11):e41914. DOI: 10.2196/41914. PMID: 36309347; PMCID: PMC9640199.
Wednesday, December 1, 2021
FMO3 and COVID-19
Individuals differ in their susceptibility to viral infections and genes contribute to the risk score. Less than 10% of humans infected with Mycobacterium tuberculosis develop TB, partially because of polymorphism in Tyrosine kinase (TYK2, P1104A) also responsible for severe COVID-19. Early in the pandemic, it was discovered that SARS-CoV-2 infection is dependent on the ACE2 receptor for cell entry and the serine protease TMPRSS2 for spike protein priming. ACE2 expression, indeed, influences COVID-19 risk and a rare variant located close to this gene was found to confer protection against COVID-19, possibly by decreasing ACE2 expression. Interestingly, FMO3 is one of the few genes with expression correlated to ACE2 [Sungnak et al, 2020] along with genes associated with immune functions.
One of the characteristics of COVID-19 is the appearance of inflammatory processes, which could be leading to increased levels of TMAO. It could contribute to the hypercoagulative state in COVID-19-associated coagulopathy (CAC). SARS-Cov2 was shown to enhance TMAO-induced inflammation.
Coronavirus disease is associated with increased risk of thrombotic events. According to recent research, low levels of FMO3 protect against thrombosis [Shih et al, 2019] while some FMO3 mutations confer higher risk [Oliveira-Filho et al, 2021]. FMO3 rs1736557 might increase the anti‐platelet efficacy of clopidogrel [Zhu et al, 2021]. Genetic risk can be mediated by gut microbiota [Gabashvili, 2020]. There are also associations with salt tolerance, wound healing, and diseases such as diabetes, renal and cardiovascular conditions increasing risk of severe COVID-19.
Studying trimethylaminuria-like conditions might help in developing strategies for prevention and therapy of other diseases, including COVID-19.
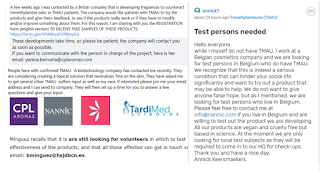
Our COVID-19 disease and vaccines study [NCT04832932, Gabashvili, 2021] compares side-effects of vaccines and clinical course of infections (including vaccine breakthroughs) in several cohorts including MEBO and TMAU. You can help by enrolling and participating in this online survey in English or Spanish.
REFERENCES
Andreakos E, Abel L, Vinh DC, Kaja E, Drolet BA, Zhang Q, O’Farrelly C, Novelli G, Rodríguez-Gallego C, Haerynck F, Prando C. A global effort to dissect the human genetic basis of resistance to SARS-CoV-2 infection. Nature immunology. 2021 Oct 18:1-6.
Gabashvili IS. Cutaneous Bacteria in the Gut Microbiome as Biomarkers of Systemic Malodor and People Are Allergic to Me (PATM) Conditions: Insights from a Virtually Conducted Clinical Trial. JMIR Dermatology. 2020 Nov 4;3(1):e10508.
Gabashvili IS. Community-Based Phenotypic Study of Safety, Tolerability, Reactogenicity and Immunogenicity of Emergency-Use-Authorized Vaccines Against COVID-19 and Viral Shedding Potential of Post-Vaccination Infections: Protocol for an Ambispective study. medRxiv 2021.06.28.21256779; doi: https://doi.org/10.1101/2021.06.28.21256779
Liu W, Wang C, Xia Y, Xia W, Liu G, Ren C, Gu Y, Li X, Lu P. Elevated plasma trimethylamine-N-oxide levels are associated with diabetic retinopathy. Acta Diabetologica. 2021 Feb;58(2):221-9.
Janmohamed A, Dolphin CT, Phillips IR, Shephard EA. Quantification and cellular localization of expression in human skin of genes encoding flavin-containing monooxygenases and cytochromes P450. Biochemical pharmacology. 2001 Sep 15;62(6):777-86.
Oliveira-Filho AF, Medeiros PF, Velloso RN, Lima EC, Aquino IM, Nunes AB. Trimethylaminuria and Vascular Complications. Journal of the Endocrine Society. 2021 Apr;5(Supplement_1):A313-4.
Zhu KX, Song PY, Li MP, Du YX, Ma QL, Peng LM, Chen XP. Association of FMO3 rs1736557 polymorphism with clopidogrel response in Chinese patients with coronary artery disease. European Journal of Clinical Pharmacology. 2021 Mar;77(3):359-68.
Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, Talavera-López C, Maatz H, Reichart D, Sampaziotis F, Worlock KB. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nature medicine. 2020 May;26(5):681-7.
Shih, D.M., Zhu, W., Schugar, R.C., Meng, Y., Jia, X., Miikeda, A., Wang, Z., Zieger, M., Lee, R., Graham, M. and Allayee, H., 2019. Genetic deficiency of Flavin-containing monooxygenase 3 (Fmo3) protects against thrombosis but has only a minor effect on plasma lipid levels—brief report. Arteriosclerosis, thrombosis, and vascular biology, 39(6), pp.1045-1054.
Tuesday, January 26, 2021
Rebuild your Health
There is increasing evidence that intestinal microbial dysbiosis has a role in the pathogenesis of systemic malodor conditions and other metabolic disorders. The most studied non-syndromic malodor condition Trimethylaminuria is usually inherited in an autosomal recessive fashion, which means that two mutations from both parents, both affecting abilities of FMO3 enzyme to catalyze the N-oxidation of trimethylamine into trimethylamine (eg, [Glu158Lys (rs2266782) and Glu308Gly (rs2266780)]), may be needed for a person to have symptoms. Yet genotype is not always predictive of phenotype, not even in this case.
 |
| Illustration by Monica Garwood |
Studies have shown that the symptoms of metabolic inefficiencies, food intolerance and even allergies can be relieved by changing the composition of intestinal microbes and adjusting dietary components feeding these microbes - to encourage growth of microorganisms properly digesting problem ingredients. Lactose-digesting bacteria Lactobacillus acidophilus, Lactobacillus bulgaricus and Streptococcus thermophilus, for example, can help to digest lactose into useful compounds, instead of offensive gas. On the other hand, the low-FODMAP diet reduces gastrointestinal symptoms by reducing the food that bacteria ferment. For lactose-intolerance, however, the "O" in FODMAPs - oligosacharides - can be beneficial as Galacto-oligosaccharides (GOS) are useful prebiotics promoting the growth of the right microorganisms.
Rebuilding the network of microorganisms on and inside our bodies can help to improve the volatiles in the surrounding air, aka body and breath odor. Microbes associated with unpleasant odors include Anaerococcus, Corynebacterium, Campylobacter, and Propionibacterium [1], Gardnerella, Alloprevotella, Sutterella, and species of Candida. Microbes associated with improvements in odors include archaebiotic Methanomassiliicoccus luminyensis, Lactobacillus pentosus KCA1, and Lactobacillus salivarius, but there are more, working together and relying on each other. Our studies (see protocols of microbiome [2] and volatilome [3] trials published on Medrxiv) identified several microbial strains and volatile compounds associated with improvement of malodor symptoms. We are currently summarizing our results and plan to publish it. Development of personalized protocols and defining the right compositions of probiotics and prebiotics is a long-term research endeavor. Meanwhile, be your own best medical researcher and take control of your wellbeing:
Step 1: Pull out your fitness journal and create an action plan
- Analyze your diet, everyday activities, exercise and sleep patterns to make initial guesses about things that could be triggering your flareups or making you feel better. Write out a list of these things.
- Break your goal into small steps and milestones. For example: if you have fructose as a potential trigger on your list, go fructose free for a week. An earlier survey of about 100 body odor and halitosis sufferers indicated stress (34%), food (25%) and environment, including the weather and perfumed products (15%) as main triggers of odors or PATM. Make sure you are not missing something in your diet - like Zinc, Vitamin C, or Vitamin D - insufficient amounts of these vitamins and minerals could also contribute to PATM.
- Develop metrics for evaluating progress. Some people can't objectively evaluate their malodor or PATM condition. Try to find a trust buddy or take note of how the people around you react when you’re in close proximity. For example, pay attention to the space people leave between you and themselves (assuming COVID-19 is behind us and the 6-feet rule no longer applies!)
- Intestinal lining is regenerating every five to seven days, so you need to stick to your diet for at least a week to notice improvements in your symptoms. Most elimination diets are actually recommended for about 3–6 weeks, to allow the antibodies (negatively reacting to problem food components) dissipate. So if your diet seems to be helping, extend it to 3 or 6 weeks.
- If it is not helping, try the next thing on your list. It should not be just diet - one study showed that bad breath was associated with abnormal sleep patterns. Perhaps you need to reevaluate your clothing material, temperature an humidity or mycotoxins in the environment? Are you getting enough sunlight ? Does your home have a healthy microbiome? Try to eliminate the triggers one at a time. No need to reduce your overall food intake, many people observe malodor or PATM flareups when they are hungry & undernourished. Try to train your body to digest more fiber - but start adding them to your diet little at a time, on weekends when you can safely experiment.
Step 3: Let go of past hurts
- Stop dwelling on the past. You have the power to change your future. Learn how to express confidence with your body language. Pretend you are comfortable in presence of other people and they will learn to be comfortable in yours.
RFRERENCES
1. Gabashvili IS. Cutaneous Bacteria in the Gut Microbiome as Biomarkers of Systemic Malodor and People Are Allergic to Me (PATM) Conditions: Insights From a Virtually Conducted Clinical Trial. JMIR Dermatology. 2020 Nov 4;3(1):e10508.
2. Gabashvili I.S. Dynamics of the Gut Microbiota in MEBO and PATM conditions: Protocol of a fully remote clinical study. medRxiv. 2020 Aug.24. medRxiv 2020.08.21.20179242; doi: https://doi.org/10.1101/2020.08.21.20179242
3. Gabashvili I.S. Effects of diet, activities, environmental exposures and trimethylamine metabolism on alveolar breath compounds: protocol for a retrospective case-cohort observational study medRxiv 2021, Jan. 26 2021.01.25.21250101; doi: https://doi.org/10.1101/2021.01.25.21250101
Friday, October 23, 2020
The Many Genes of TMAU
Twenty years ago Trimethylaminuria was linked to mutations in the FMO3 gene. It turns out there are many more genes that can lead to this condition.