Our preliminary results, based on responses to the survey for 24 members of MEBO community and 6 of their family members show a wide variety of reactions to Astrazeneca, J&J, Moderna, Pfizer and Sinovac/Coronavac vaccines.
Interestingly, Pfizer vaccine that caused no or very mild reactions in several MEBO participants, was also the vaccine that possibly caused temporary worsening of odor symptoms in one person in the community. Another MEBO participant that reported possible worsening of odor from Moderna vaccine had one thing in common with the other individual - they both had pre-existing conditions related to their upper digestive tract. Some Astrazeneca recipients also reported odor issues but did not think it was worse than usual.
One of the most interesting observations was that even though only 2 members of MEBO/PATM community reported COVID-19 infection (before or between vaccinations), both of them had long COVID with long-term neurological manifestations such as fatigue, ENT symptoms and loss of smell.
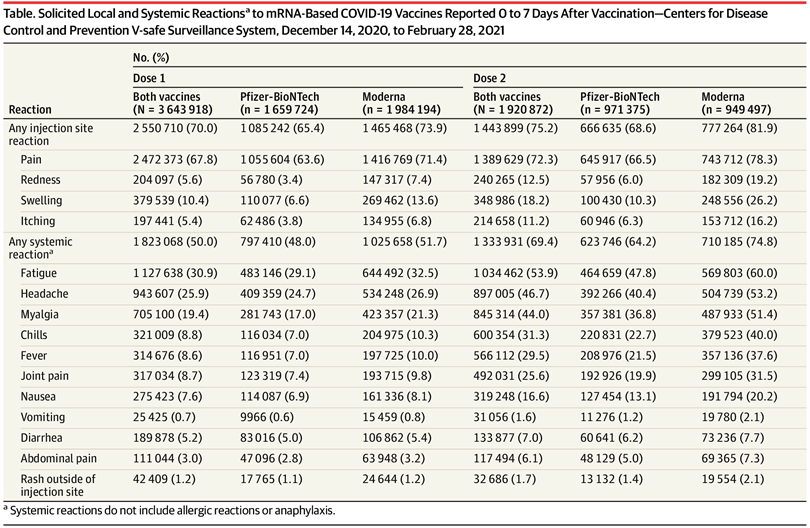
Adverse reactions to COVID-19 vaccines are influenced by a multitude of factors, many of which can be anticipated and alleviated. A certain level of inflammation is needed to trigger an effective adaptive immune response, but both environment and genetic makeup determine who is more likely to experience particular symptoms after infection and from the vaccine.
You can help by telling us about your experiences with COVID-19 and/or vaccinations. These surveys can be used for posting your brief stories - no need to answer all the questions. And you can always add to your story later. Please use your anonymous ID and let us know if you have any questions.
Survey
in English: https://bit.ly/BTN-eng
en Español: https:/bit.ly/BTN-esp
We'll be posting more observations and comparisons with over 600 participants of our study from other communities.
REFERENCES
Blumental S, Debré P. Challenges and issues of anti-SARS-CoV-2 vaccines. Frontiers in Medicine. 2021;8.
Gordon AR, Kimball BA, Sorjonen K, Karshikoff B, Axelsson J, Lekander M, Lundström JN, Olsson MJ. Detection of inflammation via volatile cues in human urine. Chemical senses. 2018 Nov 1;43(9):711-9.
Kimball BA, Opiekun M, Yamazaki K, Beauchamp GK. Immunization alters body odor. Physiology & behavior. 2014 Apr 10;128:80-5.