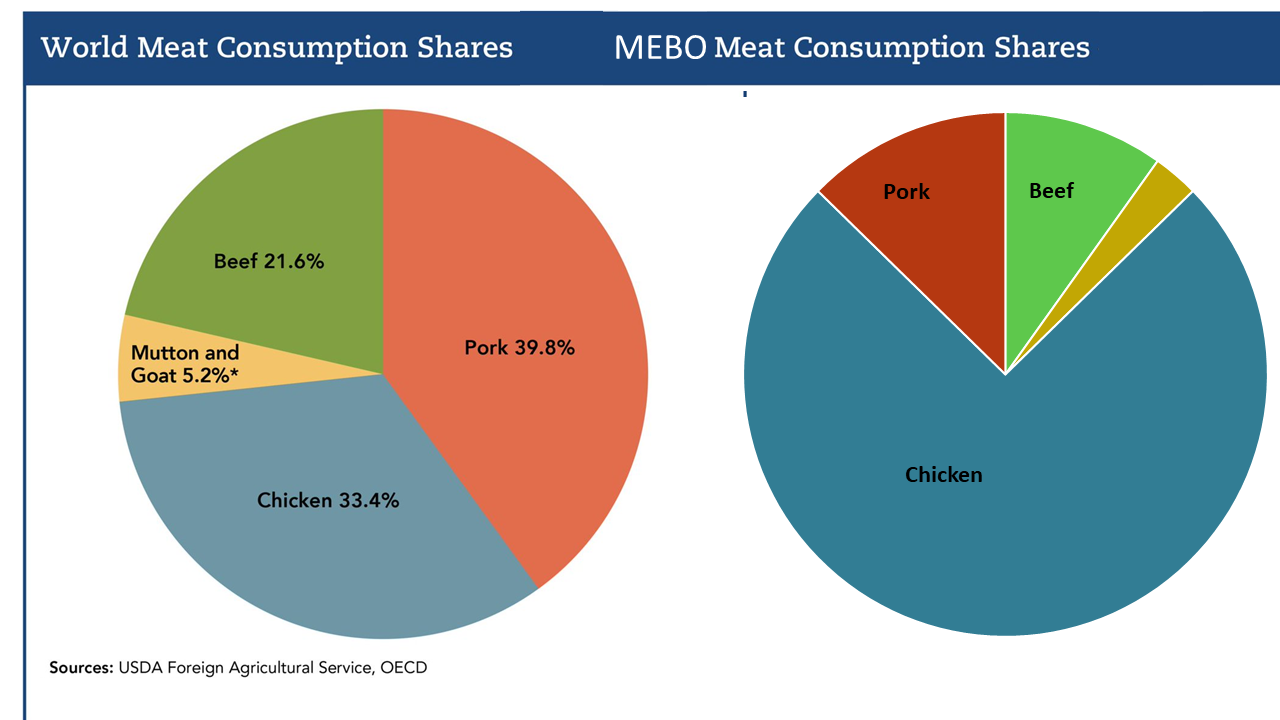
This week's TL;DR: Diets that are high in fiber and lower in animal protein, plus Mediterranean-style eating, are emerging as the most food-first ways to reduce gut production of trimethylamine (TMA) and its oxidized form TMAO. Early evidence also points to targeted botanicals and postbiotics as promising add-ons - especially for people with heart or kidney concerns. If you live with MEBO/TMAU, the same general principles may apply.
What seems to help most
1) High-fiber, lower-protein patterns (especially for CKD).
A fiber-rich, modest-protein intake can rebalance gut microbes and lower circulating TMAO in chronic kidney disease. Think: loads of vegetables, legumes, whole grains, nuts/seeds—while keeping total protein moderate and favoring plant sources. (Udomkarnjananun et al., 2025)
2) Mediterranean diet (MED).
A short, 4-week MED intervention—vegetables, fruits, legumes, whole grains, olive oil, nuts; limited red/processed meat—significantly reduced blood TMAO, even in healthy adults. Men in the study also saw better lipids and anthropometrics. (Deniz & Baş, 2025)
Since fish contains pre-formed TMAO that can worsen odor in TMAU, adapt a fish-free Mediterranean pattern if you’re sensitive.
3) Botanicals with gut–heart effects (CHF).
In patients with chronic heart failure, the Chinese botanical formula Qili Qiangxin (QLQX) reduced BNP, TNF-α, IL-6, and TMAO, pointing to lower systemic inflammation and improved barrier function. Food pattern still matters, but this suggests a potential adjunct under medical guidance. (Zhu et al., 2025)
Qiliqiangxin consists of extracts from eleven traditional Chinese medicinal herbs including for example: Panax ginseng (ginseng), Astragalus mongholicus (Mongolian milkvetch), Salvia miltiorrhiza (red sage), Cinnamomum cassia (cinnamon twig), Aconitum carmichaelii (Chinese aconite root), Descurainia sophia (flixweed), Periploca sepium (Chinese silkvine root bark), Alisma plantago-aquatica subsp. orientale (Oriental waterplantain), Carthamus tinctorius (safflower), Polygonatum odoratum (Angular Solomon's seal), and Citrus reticulata (dried mandarin peel)
4) Postbiotics (preclinical but intriguing).
In a choline-boosted, high-fat mouse model of atherosclerosis, Weizmannia coagulans JA845 postbiotics (based on B. coagulans JA845) lowered TMAO, improved the microbiome profile, dampened JAK/STAT3 inflammation, and protected vessels. Human data are pending, but this supports the microbiome-modulation avenue alongside diet. (Ma et al., 2025)
Unlike probiotics (which are live microorganisms) and prebiotics (which are food/substrates that feed beneficial microbes), postbiotics are non-live microbial cells, microbial cell parts, or microbial metabolites (or a mix) that can have beneficial effects.
Example components might include dead/inactivated bacterial cells, cell wall fragments, microbial metabolites like short-chain fatty acids (SCFAs: butyrate, acetate, propionate), peptides and enzymes.