In the ever-evolving landscape of medical science, the untangling of medical mysteries often hinges not just on technological advancements or expert researchers, but on the active involvement of community members. Community efforts have been instrumental in the identification and understanding of elusive conditions MEBO (Metabolic Body Odor) and PATM (People Are Allergic to Me).
Late 1990s - early 2000s: The Dawn of Online Support Forums
Before the conditions were officially named, online forums like MSN Body Odor Support Forum, ibsgroup.org, Yahoo TMAU group, and Curezone BO & Halitosis and TMAU forums served as early platforms for sufferers to discuss their symptoms.
At this time, Trimethylaminuria (TMAU) was a scarcely recognized condition, and diagnostic tests were both costly and geographically limited. Trimethylaminuria support group, later established as foundation raises 35K and awards it to Dr. George Preti of Monell Center, the world’s only independent, non-profit scientific institute dedicated to interdisciplinary basic research on the senses of taste and smell.
2006-2007: Birth of MEBO and PATM Communities
In 2006, the acronym "PATM" was first coined by a sufferer, and by 2007, a dedicated PATM community was established on MedHelp. The initial post was reposted in PATM forum and garnered over 8,800 responses, signifying the start of a community-led initiative to explore the condition. While the term FBO (fecal body odor) emerged earlier and is still used on online forums, it is often avoided due to its less appealing connotation. MEBO was coined by another individual suffering from a similar undiagnosed condition. This further fueled community-driven research and knowledge sharing among those affected.
2008: Broadening the Dialogue
The blog Bloodbornebodyodorandhalitosis.com is launched, later transitioned to meboblog.com. This year also saw more in-person meetups and community surveys, including one by pharmacist Arun Nagrath that received about 100 responses. 95% of responders was trying to seek medical help, over 90% thought that their doctor was not knowledgeable nor confident in their recommendations.
2009: Formalizing Research Efforts
MEBO Research Charity was founded in both the UK and Florida, spearheaded by Maria de la Torre. The first collaborative study with UK's Biolab was initiated, focusing on blood and urine tests. The results were subsequently published on the MEBO blog and clinicaltrials.gov (
NCT02692495, principal investigator: Irene Gabashvili).
2010: Unveiling the Microbiome and Genetic Factors
At MEBO's 1st annual conference, held in Nashville, Dr. Gabashvili presents
"Microbes and us," discussing the human microbiome's role in poorly understood conditions like idiopathic malodor and multiple chemical sensitivities (MCS). Previously, MEBO interviewed
Metametrix about their GI Effects panel, which measured stool bacteria, fungus, and parasites with DNA analysis. Metametrix, pioneer in diagnostics of nutritional insufficiencies and metabolic dysfunction,was later acquired by Genova Diagnostics.
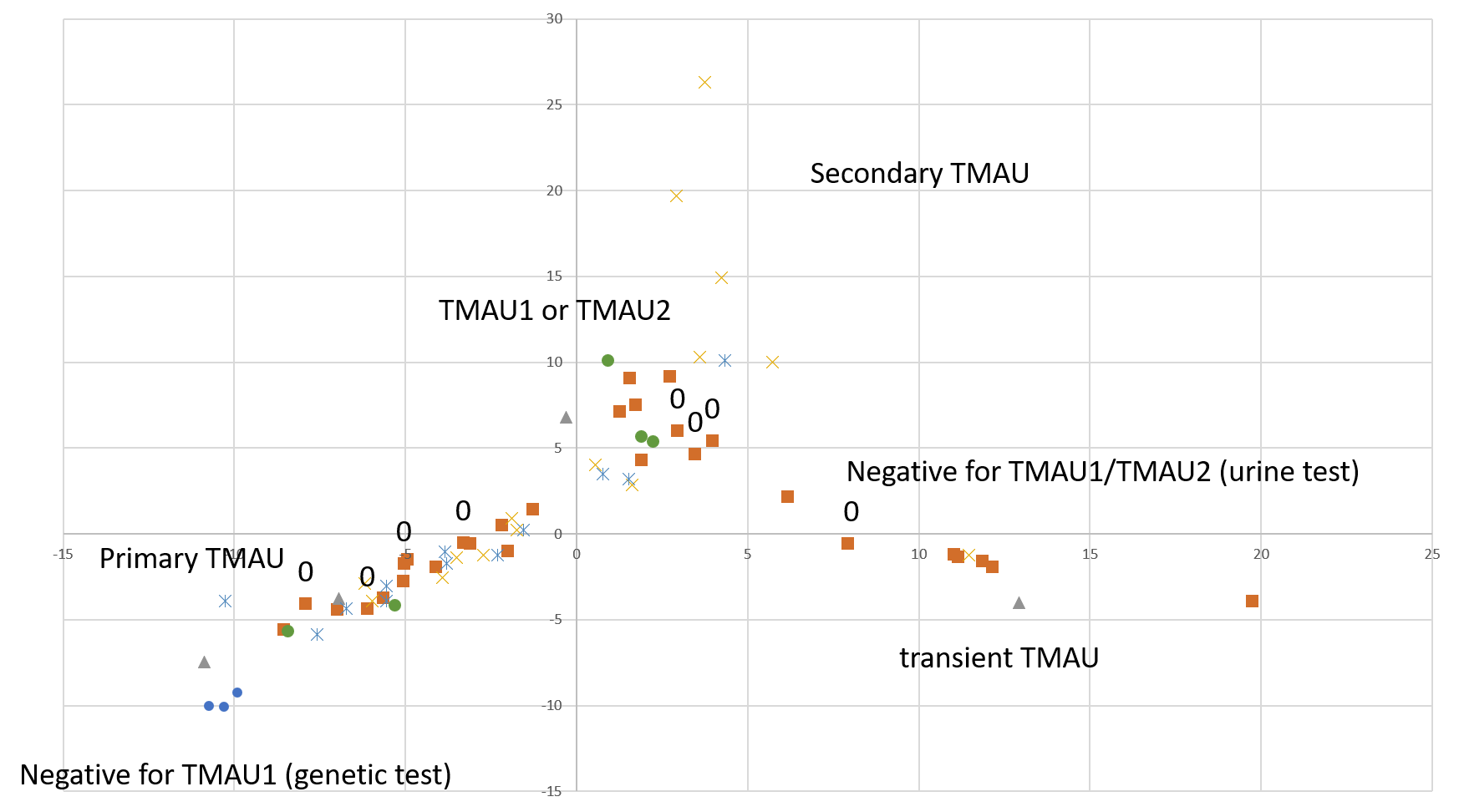
Dr. Nigel Manning introduces 12 potential subtypes of TMAU. Out of 1,150 urine samples from 716 individuals collected between 1997 and 2009, 379 (53%) indicate significant TMAU presence. The launch of a new FMO3 genetic testing service promises to provide clearer diagnostic results. Additionally, a
TMAU service dog program is initiated.
2011: The Advent of Genomic Data Sharing
The
second annual meetup in Washington, DC, focuses on the interplay between genetic mechanisms and holistic health. Skype conference call group is formed.
2012: Empowering Patients Through Technology
A new MEBO study focusing on alveolar breath is initiated (
NCT03451994). Aurametrix health management software is publicly launched, allowing patients to diagnose metabolic inefficiencies through
digital food and symptom journaling. Karen James, MEBO UK’s Public Relations Director, publishes an article in the Royal College of General Practitioners (RCGP) journal InnovAiT, describing the
life of a TMAU sufferer. For
iGEM competition, student
team from Fatih university genetically engineers bacteria producing geraniol and FMO3 to eliminate TMA odors. Their product, FreshEcoli, is supposed to work as a synthetic perfume.
The
Third Annual Meetup in Miami Beach features Dr. Elizabeth Shephard discussing pharmacogenetics and personalized medicine.
2013: Deepening Theoretical Insights
MEBO UK's scientific director, Dr. Colin Harvey-Woodworth, publishes an article proposing that some MEBO symptoms may be secondary to
dimethylsulphidemia, a previously unidentified metabolic condition linked to DMGDH gene (missense mutation in DMGDH was known to be associated with
fish odor similar to
pyridoxine non-responsive homocystinuria). Concurrently, a
mediterranean study reveals that individuals carrying FMO3 mutations may not necessarily experience odor issues. The study finds that the TMA/TMAO ratio in urine samples from individuals with 158KK/308EG variants indicates reduced FMO3 activity, yet these individuals do not exhibit the hallmark fish-like odor commonly associated with trimethylaminuria. This data underscores the notion that the expression of trimethylaminuria symptoms is influenced by factors beyond the presence of specific genetic variants.
2014: Therapeutic Innovations
2015: Expanding Testing and new molecular targets
3,3-Dimethyl-1-butanol (DMB), which is a structural analog of choline found in some foods, such as balsamic vinegars, red wines, some cold-pressed extra virgin olive oils and grapeseed oils
is demonstrated to inhibit TMA production by gut bacteria. DMB has potential as a therapeutic approach. Studies also show the inhibitory effects of Resveratrol on TMA production in mice, further expanding the scope of potential small molecule targets. Dr Stanley Hazen files
a patent.
2016: Streamlining Diagnostic Approaches
MEBO collaborates with
Professor David Wishart on a Urine Metabolomics study, registered as
NCT02683876, involving Canadian participants. The study aims to explore simpler, non-challenge-based tests for diagnosis.
Several sufferers in the MEBO community
report taking Resveratrol for a few months, with excellent results in decreasing or completely eliminating their odor symptoms while increasing consumption of foods high in choline, carnitine, and lecithin.
2017: Diagnostic Breakthroughs and the Social Media Shift
MEBO's Scientific Director, Irene Gabashvili, publishes the
Biolab study on BiorXiv. The study reveals significant differences in intestinal permeability among participants based on body regions responsible for VOC emissions. In addition, the study identifies two subgroups of MEBO/PATM sufferers based on sugar intake. Due to the small sample size of 16 participants, the article remains a preprint. Unfortunately, the current structure and incentives of mainstream academic publishing favor well-funded research on common diseases and are less accommodating to research on overlooked rare conditions.
A
Monell Center Study published in BMC Medical Genetics delves into the genetic complexities of TMAU, revealing that not all cases are linked to the FMO3 gene. Although the choline challenge test confirmed a diagnosis of TMAU by revealing a high level of urinary TMA in all 10 subjects, genetic analyses revealed that the FMO3 gene appeared to be normal in four of the 10. Additional analyses revealed defects in several other genes that could contribute to the inability to metabolize the odorous TMA. No rare variants are found in PYROXD2 and a DMGDH, but there were associations with BHMT2, SARDH and SHMT1 genes, which directly interact with DMGDH in the gene network and may participate in the same pathway. At MEBO conference in Miami Beach, Professor Shephard talks about
microbiome and diet.
Danny Kunz and his Citizen Research Group in Germany initiate a DNA sequencing study. Their simulations backed by large enzyme databases suggest that Thyroid-stimulating hormone (TSH) may play a role. Danny proposes a new name for the condition: Intestinal Metabolic Bromhidrosis Syndrome (IMBS).
TMAU UP Podcast is launched on YouTube. Facebook's "Groups" feature spurs the creation of new private MEBO and PATM communities, marking a new era in community engagement and data sharing.
2018-2020: Advancing Research and Understanding
A Japanese paper confirms
PATM as a physical condition connected to skin petrochemicals and microbes. Meanwhile a case report entitled "People allergic to me and body dysmorphic disorder" published in Asian Journal of Psychiatry is linking a case to a relatively common psychiatric disorder characterized by preoccupations with perceived defects in physical appearance. The average age of BDD onset was previously estimated as 15 with symptoms lasting 18 years on average without proper treatment. The prevalence of BDD is thought to be 0.7-2.4% in the general population, but the condition remains underdiagnosed and poorly understood.
Results from the
MEBO-Wishart study align with previous MEBO/PATM findings but highlight the limitations of morning urine tests. A new PATM survey is conducted by an independent PATM ufferer/researcher. Average age of responders is 28. Mononucleosis due to CMV is proposed as the cause of PATM.
A
UC San Diego student team explores the enzymatic breakdown of TMA. New gene
SELENBP1 is proposed to explain metabolic halitosis. A patent on using Mikania plant extract to inhibit the conversion of choline to trimethylamine (TMA) is
filed and granted, based on an
earlier patent for using this plant to suppress body odor.
RareConnect is established as a platform for those affected by rare diseases, including MEBO Research members. MEBO Research becomes a member. Unfortunately, by the end of 2023 it will be shut down, not being able to compete with Facebook and Reddit. Yahoo Groups shut down on December 15, 2020, for the same reason. New Instagram and WhatsApp groups are created.
New paper "
Treatments of trimethylaminuria: where we are and where we might be heading" is published. It reviews Fecal microbial transplantation (FMT) that was
not especially successful for reducing TMA or was only transiently effective as the
symptoms returned one year after treatment. Antibiotic treatment is also transiently effective in some patients and completely ineffective in others. Future research directions include gene therapy, enzyme replacement/enhancement therapy and gut microbiome modulation.
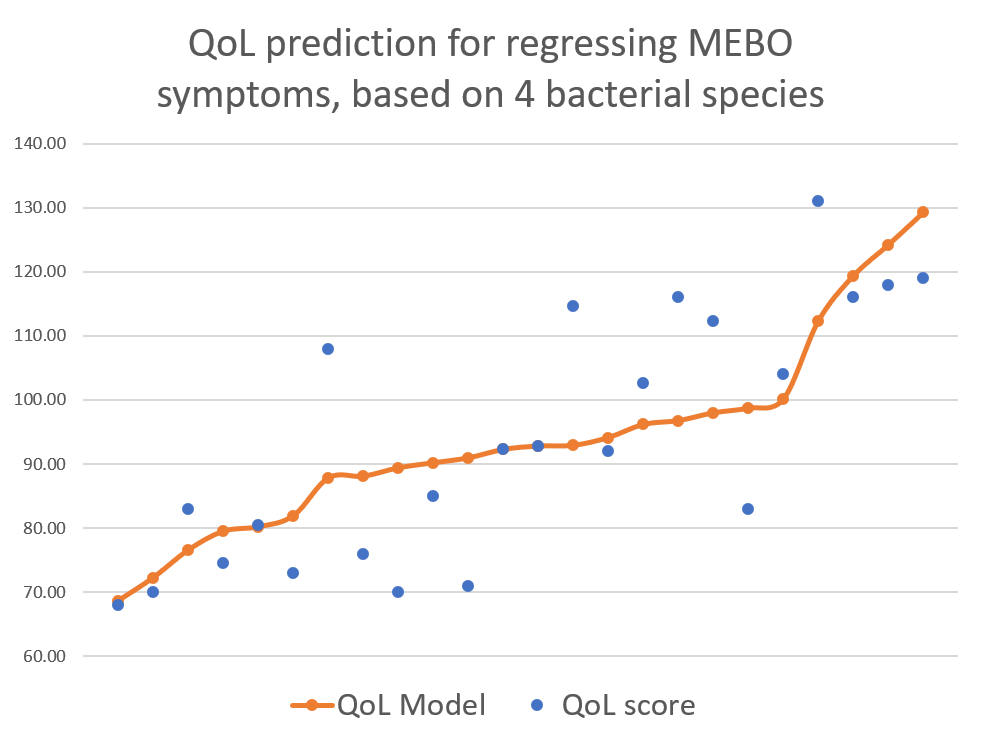
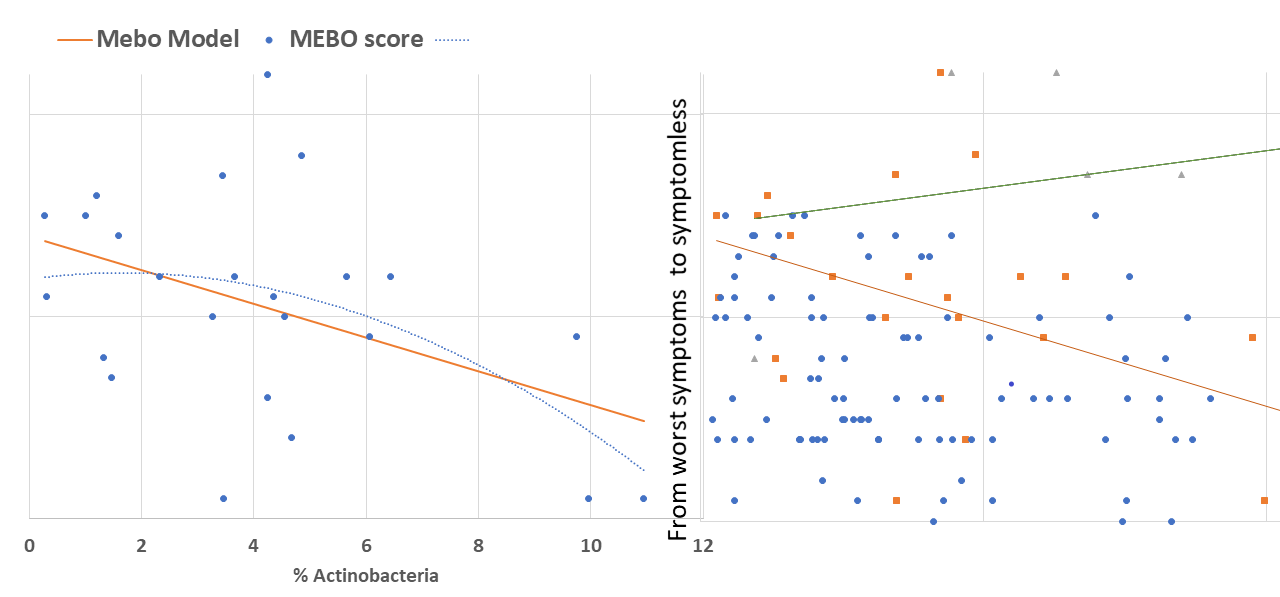
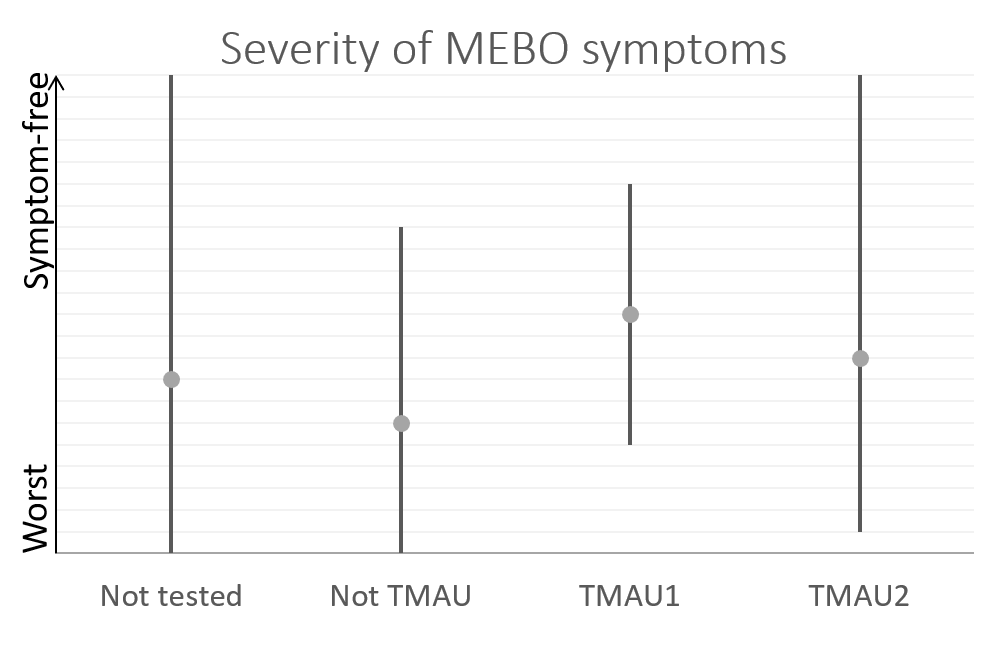
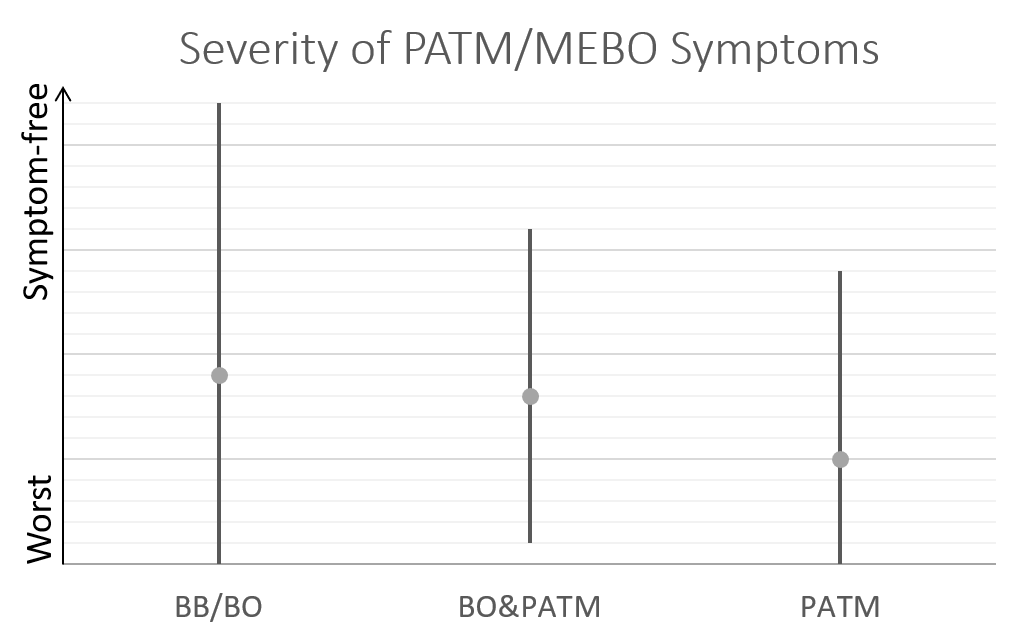
Peer-reviewed paper examining the microbiome traits of individuals self-identifying with PATM and MEBO (NCT02683876) is published in JMIR Dermatology. The study reveals that both MEBO and PATM share increased levels of malodor-associated skin bacteria compared to non-MEBO/non-PATM groups, correlating with severity of self-reported symptoms. However, both populations exhibit significant heterogeneity.
2021-2023: Ongoing Challenges and Future Directions
A COVID study identifies flare-ups in 10-15% of the MEBO population post-infection and vaccination, possibly related to microbiome and hormonal fluctuations (NCT04832932; peer-reviewed paper published in JMIR Formative Research). COVID-19 has led to the emergence of new cases, with individuals developing MEBO/PATM conditions following infection and/or vaccination.
A cysteine challenge test for hydrogen sulfide production is suggested. Florida State University's iGem team proposes a synthetic biology project for TMAU.
New paper by Chris Callewaert explores various cutting-edge approaches to skin health, including genetically engineered probiotics and microbiome transplantation. While promising, the latter method currently lacks scalability for industrial applications. The paper also delves into skin bacteriotherapy, a technique involving the application of one or multiple pure bacterial cultures with health-promoting properties to cleansed or disinfected skin areas. Additionally, the study examines the use of prebiotics applied directly to the skin to encourage the growth of beneficial microbes. Each of these innovative approaches holds promise but also presents its own set of challenges.
A study by Professor Sekine in Nature Scientific Reports identifies volatile organic compounds as key differentiators between PATM sufferers and controls. These results align with our yet to be published findings from MEBO-Menssana Alveolar Breath Test Study (NCT03451994) and Microbiome study (NCT03582826).
The FSU team introduces their innovative probiotic, E.esperance, at the iGEM competition in Paris on November 2, 2023.
Despite these advancements, mainstream science remains largely uninterested in community-based research, leaving MEBO, PATM and TMAU without a definitive cure.