Every infection has a distinct odor. It could be associated with changes in the gut microbiome. Besides, circulating B-cells from our immune system are also producing chemical odors that appear after viral infection. T-cell and cytokine involvement is also possible. Infections can change body odor for the worse. PATM or MEBO conditions could begin after an infection and linger thereafter.
COVID-19 is known to be associated with a specific odor. Early studies identified volatile compounds that discriminated COVID-19 from other conditions. Some of these compounds - such as fruity smelling ketones - are also associated with diabetes - a risk factor for Severe COVID-19 infection. Another compound, Heptanal, associated with lung cancer, can also predict the severity of the Coronavirus disease.
Dogs (and rats and other animals) can easily detect the smell of COVID-19. They are already helping during this pandemic - Massachusetts schools, for example, are using dogs to sniff out Covid-19. The dogs come to the schools weekly and work to detect cases in empty classrooms, auditoriums, cafeterias and gymnasiums, If Covid is detected, the authorities tell the health nurse who relays the information to the people affected.
Long COVID - when people continue to have symptoms of COVID-19 for months after their initial illness. - has a distinct smell as well. A paper posted today on MedRxiv tells that dogs can easily detect long COVID as well - in at least half of the cases.
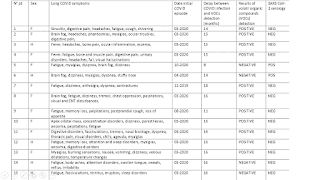
Between May and October 2021, 45 Long COVID patients sent their axillary sweat samples to the National Veterinary School of Alfort. Average age of the patients was 45 (6-71) and 73.3% were female. No patient had been admitted in intensive care unit during the acute phase. Prolonged symptoms had been evolving for an average of 15.2 months (range: 5-22). Main symptoms of prolonged phase were intense fatigue (n=37, 82.2%), neurocognitive disorders such as concentration and attention difficulties, immediate memory loss (n=24, 53.3%), myalgias/arthralgias (n=22, 48.9%), cardiopulmonary symptoms (dyspnea, cough, chest pain, palpitations) (n=21, 46.7%), digestive symptoms (diarrhea, abdominal pain, reflux, gastroparesis...) (n=18, 40.0%), ENT disorders (hyposmia, parosmia, tinnitus, nasal obstruction, inflammatory tongue, dysphonia, sinusitis) (n=18, 40.0%) (table 1). 11 (24.4) patients had at least one positive SARS-CoV-2 serology before any vaccination, 29 (64.4%) had a negative SARS-CoV-2 serology and 5 (11.1%) had no serology results. Snapshot of the table shows some of the cases. Interestingly, patients with odor exhibited symptoms similar to long COVID sufferers in the MEBO community. This includes loss of smell and heart palpitations.
REFERENCES